2019
Year 39

Prof. Helen S. Mayberg
Director of The Center for Advanced Circuit Therapeutics
Mount Sinai Health System, New York, USA
RETHINKING DEPRESSION AND ITS TREATMENT - STIMULATING THE BRAIN TO HEAL THE MIND
Dr. Mayberg received an MD from the University of Southern California. She trained at the Neurological
Institute of New York at Columbia University and was a post-doctoral fellow in nuclear medicine at Johns
Hopkins Medicine. Immediately prior to joining Mount Sinai, Dr. Mayberg was Professor of Psychiatry,
Neurology, and Radiology and held the inaugural Dorothy C. Fuqua Chair in Psychiatric Neuroimaging and
Therapeutics at Emory University School of Medicine. She is a member of the National Academy of Medicine,
The American Academy of Arts and Sciences and the National Academy of Inventors. As Director of The
Center for Advanced Circuit Therapeutics at Mount Sinai, Dr. Mayberg builds a cross-disciplinary platform for
collaborative translational research that will bring together clinical colleagues in neurology, neurosurgery, and
psychiatry with experts from neuroscience, imaging, engineering, bioinformatics, neuro-engineering, and
computational neuroscience to foster the development of new circuit-based strategies and delivery of
state-of-the-art individualized treatments for patients with advanced neuropsychiatric disorders.
RETHINKING DEPRESSION AND ITS TREATMENT -
STIMULATING THE BRAIN TO HEAL THE MIND
Prof. Helen Mayberg delivered the 39th TS Srinivasan Endowment Oration, titled ‘Rethinking Depression and
its Treatment - Stimulating the Brain to Heal the Mind’. Prof. Mayberg led the ground-breaking research for
the treatment of depression by combining new technologies with enhanced imaging techniques. As her
research focuses upon using Deep Brain Stimulation (DBS); she explained DBS, involves implanting a small
neurostimulator/electrode into a patient’s brain to send out electrical impulses to specific brain regions. The
approach is approved by the US Food and Drug Administration to treat epilepsy and Parkinson’s disease,
among other conditions, but has long been controversial in depression treatment due to mixed findings of
the treatment’s effectiveness in the last couple of decades.

Depressed DBS patients typically have failed to respond to antidepressant medicines and psychotherapy, as
well as electroconvulsive therapy (ECT); which is usually given as a last resort to patients with major
depression who have not responded to multiple treatments. However, ECT has side effects, including
short-term memory loss in some patients.
In 2005, Dr. Helen Mayberg and her colleagues led the first trial for treatment-resistant major depression. DBS is a pioneering experimental treatment for “refractory” patients–those who have not responded to other therapies. The procedure involves surgical implantation of paired electrodes (one in each hemisphere of the brain) into a region called Area 25, which is located in the sub-callosal cingulate cortex or SCC, near the center of the brain. Those tiny electrodes are designed to deliver a small amount of current to Area 25, with the amount and frequency of the pulses fine-tuned both during and after surgery. The device, which runs on a battery that can be replaced every few years, can remain in a patient indefinitely. Many have lived with the implants, depression-free since the first DBS operations performed over a dozen years ago.
Although Dr. Mayberg is quick to acknowledge that “we still don’t know how DBS works,” when it succeeds in bringing a deeply depressed patient from out of the depths, she suspects it does so by harmonizing communications between parts of the brain that her research has shown to be out of synch. DBS, like other forms of treatment for depression, addresses all the major symptoms: depressed mood, irritability, irregular sleep, loss of motivation, and the inability to experience a pleasure. “The whole syndrome recovers,” says Prof. Mayberg. It can be extremely dramatic in some patients, while in others it takes time to become evident–as much as a year or two. Other patients appear not to be helped by DBS, for reasons that are still unclear.
In 2005, Dr. Helen Mayberg and her colleagues led the first trial for treatment-resistant major depression. DBS is a pioneering experimental treatment for “refractory” patients–those who have not responded to other therapies. The procedure involves surgical implantation of paired electrodes (one in each hemisphere of the brain) into a region called Area 25, which is located in the sub-callosal cingulate cortex or SCC, near the center of the brain. Those tiny electrodes are designed to deliver a small amount of current to Area 25, with the amount and frequency of the pulses fine-tuned both during and after surgery. The device, which runs on a battery that can be replaced every few years, can remain in a patient indefinitely. Many have lived with the implants, depression-free since the first DBS operations performed over a dozen years ago.
Although Dr. Mayberg is quick to acknowledge that “we still don’t know how DBS works,” when it succeeds in bringing a deeply depressed patient from out of the depths, she suspects it does so by harmonizing communications between parts of the brain that her research has shown to be out of synch. DBS, like other forms of treatment for depression, addresses all the major symptoms: depressed mood, irritability, irregular sleep, loss of motivation, and the inability to experience a pleasure. “The whole syndrome recovers,” says Prof. Mayberg. It can be extremely dramatic in some patients, while in others it takes time to become evident–as much as a year or two. Other patients appear not to be helped by DBS, for reasons that are still unclear.
She has been deeply moved by both successes and failures, characteristically determined to learn from all
outcomes. She has learned that even when DBS enables a patient to return to a life without debilitating
depression, other facts of life impinge. “We can change your brain,” she says, ”but we can’t change your
life.”
She says that DBS seems to allow patients to tolerate stress differently once they have recovered, and the longer they continue with DBS. But it is those patients who have achieved a sustained remission after many years of disability who remind Mayberg that all of her efforts to optimize DBS and bring it safely to more people are more than worthwhile.
Prof. Mayberg currently focusing upon how certain patients evolve over time: those who transition from responding well to standard treatment to being treatment-resistant. The central thought in this hypothesis is that depression, perhaps like other illnesses such as multiple sclerosis, comes in a few different types. Some patients get very sick and never recover; some get sick, then recover, but then relapse. In depression, Prof. Mayberg speculates that some patients, over the course of the illness, pass a point at which a transition in the brain occurs, which she likens to a phase shift. Despite past success with treatment, a patient relapses and then can no longer respond even to treatments like ECT.
Researchers are testing the hypothesis that patients who respond only partly to depression therapy of any type–who continue to have symptoms even when their mood is generally much better after treatment–may be at increased risk to eventually develop treatment resistance. “Residual” symptoms include anxiety or disturbed sleep or even moderately low mood, and diminished interest in life. Using data from imaging, her research group is trying to test this concept, looking for evidence of progressive changes in brain circuits in patients over time, to see if such changes correlate with the development of treatment resistance.
“The brain, even when it is well, is not stable,” Mayberg notes. “We have to characterize the steps of evolving resistance to treatment. Our trajectory of treatment may need to be different. This is why we have to work harder than ever to get at the origins of depression.”
She says that DBS seems to allow patients to tolerate stress differently once they have recovered, and the longer they continue with DBS. But it is those patients who have achieved a sustained remission after many years of disability who remind Mayberg that all of her efforts to optimize DBS and bring it safely to more people are more than worthwhile.
Prof. Mayberg currently focusing upon how certain patients evolve over time: those who transition from responding well to standard treatment to being treatment-resistant. The central thought in this hypothesis is that depression, perhaps like other illnesses such as multiple sclerosis, comes in a few different types. Some patients get very sick and never recover; some get sick, then recover, but then relapse. In depression, Prof. Mayberg speculates that some patients, over the course of the illness, pass a point at which a transition in the brain occurs, which she likens to a phase shift. Despite past success with treatment, a patient relapses and then can no longer respond even to treatments like ECT.
Researchers are testing the hypothesis that patients who respond only partly to depression therapy of any type–who continue to have symptoms even when their mood is generally much better after treatment–may be at increased risk to eventually develop treatment resistance. “Residual” symptoms include anxiety or disturbed sleep or even moderately low mood, and diminished interest in life. Using data from imaging, her research group is trying to test this concept, looking for evidence of progressive changes in brain circuits in patients over time, to see if such changes correlate with the development of treatment resistance.
“The brain, even when it is well, is not stable,” Mayberg notes. “We have to characterize the steps of evolving resistance to treatment. Our trajectory of treatment may need to be different. This is why we have to work harder than ever to get at the origins of depression.”


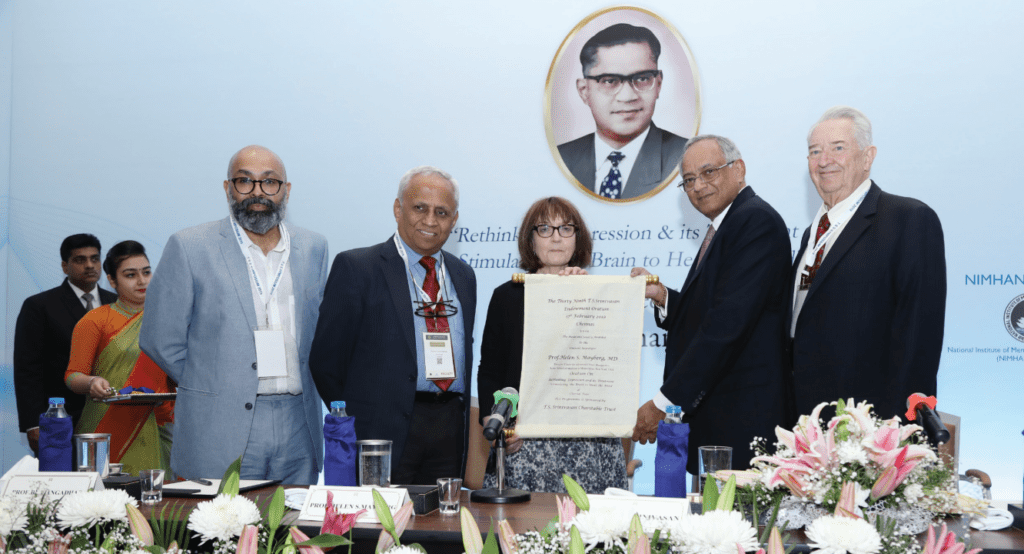
The T S Srinivasan Oration and award is sponsored by the T S Srinivasan Charitable Trust. On the occasion of
the endowment lecture, Mr. Venu Srinivasan, Chairman, TVS Motor Company, presented the T.S. Srinivasan
Gold Medal and Silk Scroll to Prof. Helen Mayberg. Prof. B.N. Gangadhar Director NIMHANS, presented the
highlights of TS Srinivasan – NIMHANS Knowledge Conclave held in NIMHANS, Bengaluru. Prof. Timothy
Pedley Professor of Neurology and Chairman Emeritus of the Department of Neurology at Columbia
University was also present during the occasion. The TS Srinivasan oration, which has traditionally featured
world leaders in neurology as orators, is attended by over 500 medical professionals and researchers from
India and abroad, medical and allied health science students and the elite of Chennai, a much-anticipated
annual event.